
Expectable Fatalities and Hospital Admissions Are Dramatized as COVID-19 Emergency
KARSTEN MONTAG, 24. Mai 2021, 0 Kommentare, PDFNote: This article ist also available in German.
In its weekly report on May 21, 2021, the German equivalent of the CDC, the Robert Koch Institute (RKI), reported a total of 83,602 COVID-19 victims in Germany. About 74,000 of them occurred during the 2020/21 flu season alone. These numbers, which are constantly repeated in the media, sound very threatening. In contrast, according to the RKI, an estimated 25,000 people died of influenza in the 2017/18 flu season.
At first glance, COVID-19 appears to be about three times more dangerous as a severe seasonal flu in Germany. But a comparison of the weekly course of age-specific mortality rates during the flu season 2020/21 with previous years shows no particular deviations, except that the peak in the flu season 2020/21 was recorded around the turn of the year, while in previous years it took place at the end of winter.
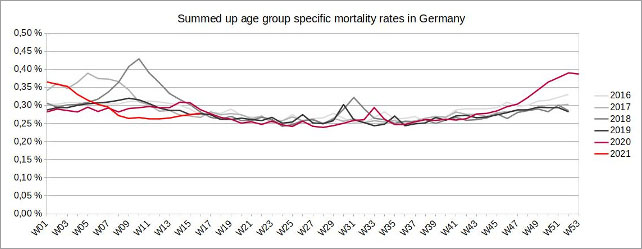
Figure 1: (click here for a larger display) Illustration by the author, data source: European Statistical Office. In order to include demographic changes, the weekly age-specific mortality rates were added up in this chart.
In fact, during the 2020/21 flu season in Germany, in all age groups fewer people died in relation to the size of their respective age group than in the 2017/18 flu season.
Where do more than 74,000 COVID-19 victims in the 2020/21 flu season in Germany come from?
Looking at the annual numbers of total mortality in Germany, a steady increase with slight fluctuations since the beginning of the millennium can be noticed.
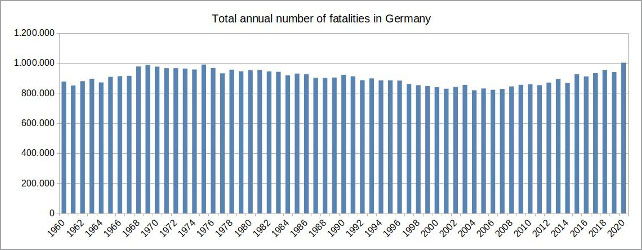
Figure 2: (click here for a larger display) Illustration by the author, data source: European Statistical Office
The reason for the increasing numbers, however, is not related to more dangerous illnesses or other external circumstances, but is simply based on the fact that the German population, like in many other western countries, is getting older and life expectancy cannot be increased indefinitely.
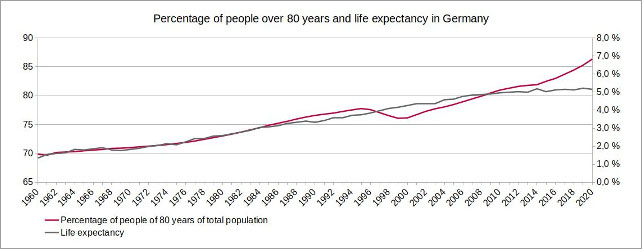
Figure 3: (click here for a larger display) Illustration by the author, data source: European Statistical Office
Improved living conditions, a healthier way of life and advances in medicine have led to an increase in life expectancy, especially in the 20th century. However, since the beginning of the 2010s, average life expectancy has not increased at the same rate as in previous decades. At the same time, the age group of people over 80, due to high birth rates at the end of the 1930s and the beginning of the 1940s, is currently growing much faster in Germany than it has just a few years ago.
The risk of dying from typical age-related diseases, or acute respiratory syndromes in combination with these diseases, is significantly higher at an old age than at a younger age. Because of the increasing percentage of people over 80 it is possible that the age-specific mortality rates are dropping or stay the same, while the number of total fatalities is rising at the same time. Comparing the 2017/18 flu season with the same period in 2020/21 illustrates this effect very well.
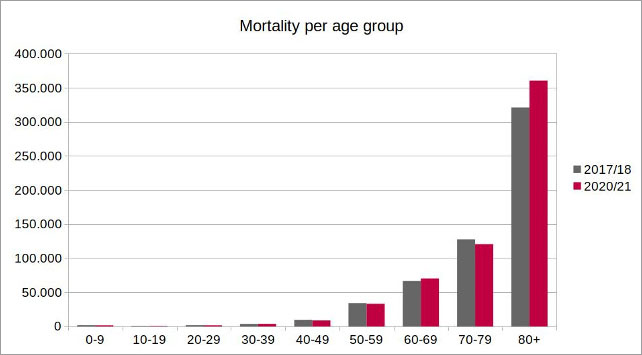
Figure 4: Illustration by the author, data source: European Statistical Office
The higher number of total fatalities in the age group of over 80 during the flu season 2020/21 in relation to the same period in 2017/18 can be clearly seen. In total, over 30,000 more deaths have occurred across all age groups.
However, since the age group of people over 80 has grown significantly in the period between these two seasons, an adequate comparison should be done by comparing the age group-specific mortality rates. Considering media’s illustration of the dramatic impact of COVID-19 in Germany, the result is rather astonishing.
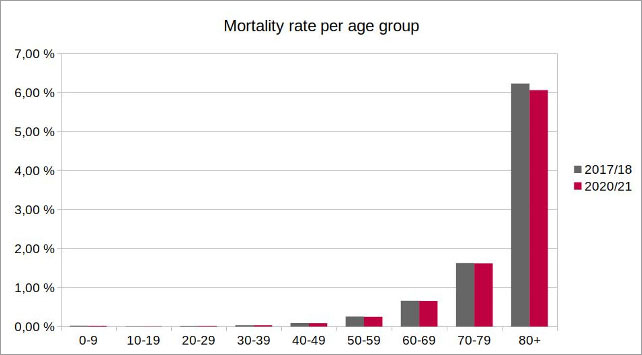
Figure 5: Illustration by the author, data source: European Statistical Office. Since the official population figures for 2021 are not yet available, a population forecast by the European Statistical Office was used to calculate the mortality rate in the 2020/21 season.
In fact, mortality rates have remained more or less the same in all younger age groups and even decreased in the age group over 80. Thus, regarding age-specific mortality rates, the COVID-19 pandemic in the 2020/21 flu season had a milder impact than the 2017/18 seasonal flu, although the total number of fatalities was significantly higher. Taking demographic changes into account, the COVID-19 pandemic in Germany has therefore so far not been more dangerous than seasonal flu epidemics.
And there is something else worth noticing. If, according to the RKI, 25,000 people died of influenza in the 2017/18 flu season and the number of total fatalities in 2020/21 was more than 30,000 higher than in 2017/18, then the number of COVID-19 victims would be just over 55,000. But RKI recorded 74,000 COVID-19-related deaths. Either RKI estimated the number of victims of the seasonal flu in 2017/18 too low, or there was an error in recording the COVID-19 fatalities. This could be explained, for example, by a large number of false positive PCR tests.
In the future, due to demographic changes, a significant increase of the total number of annual fatalities is to be expected
Due to high birth rates between 1950 and 1970, the percentage of the age group over 80 will continue to grow significantly over the next 30 years. Since life expectancy has only increased slowly over the past ten years, it must be assumed that it will grow rather moderately in the future.
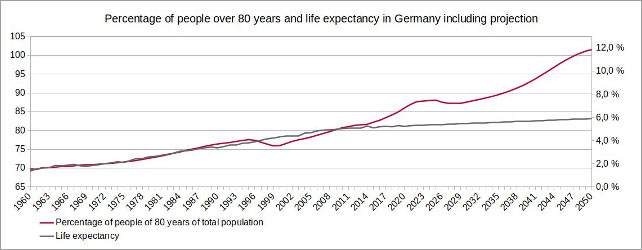
Figure 6: (click here for a larger display) Illustration by the author, data source: European Statistical Office
Even if assuming that the trend during the last ten years in declining mortality rates in all age groups will continue at a steady pace, the number of total annual fatalities in Germany is very likely to continue to grow significantly. According to the forecast, just under 40,000 more people will die in 2025 than in 2020, and in 2050 there will probably be over 200,000 more.
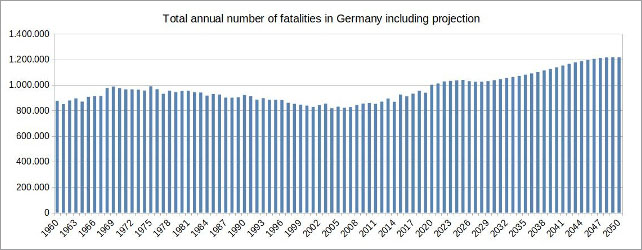
Figure 7: (click here for a larger display) Illustration by the author, data source: European Statistical Office
In order to correctly assess the danger of the coronavirus and its future mutations, it is therefore extremely important to include the demographic changes in the population. If you simply add up the absolute numbers of disease-related fatalities, a dramatic scenario arises, although the mortality rates in all age groups are actually dropping steadily.
The German health system is not designed to match the challenges of an aging society
State of emergency in hospitals. Clinic staff is absent due to illnesses. Scheduled operations need to be postponed. Health system on the edge of capacity. Hospitals and authorities paralysed. – What sounds like headlines from the COVID-19 pandemic last winter, actually happened during the peak of the flu epidemic in Germany in the beginning of 2018.
The RKI reported 25,000 victims of the seasonal flu and called it the deadliest in 30 years. It is hard to believe that, taking demographic changes into account, even in 2018 the mortality rate in Germany was lower compared to the average of previous years.
The development of hospital occupancy and demographic changes provide information about why German hospitals have reached their capacity limits so quickly in recent years during the seasonal flu. Because the average period of stay in hospital has halved since the 1990s, the number of days patients stay in hospital has dropped significantly, despite an aging population in Germany.
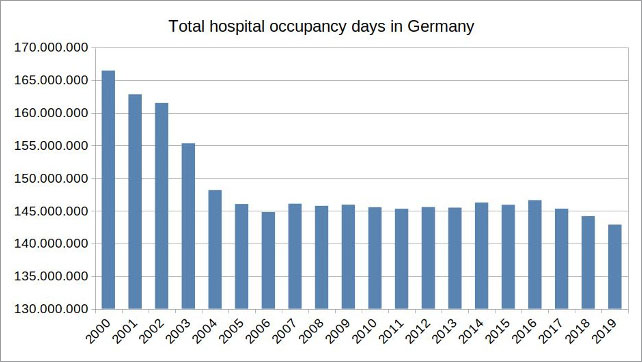
Figure 8: Illustration by the author, data source: Federal Statistical Office
Since hospitals are one of the largest cost factors in the health system, this has resulted in a reduction of overcapacities. Some hospitals have closed down permanently and the number of hospital beds has decreased by 20 percent over the past three decades.
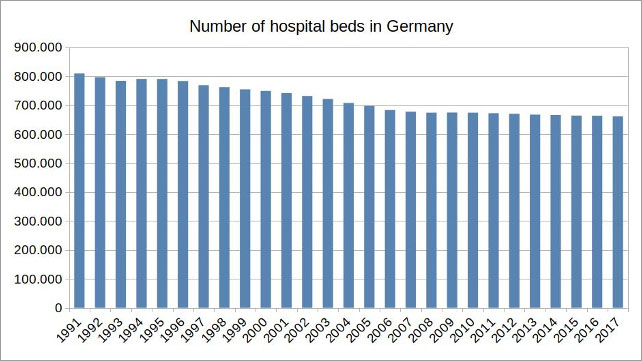
Figure 9: Illustration by the author, data source: European Statistical Office
Despite dropping overall hospitalisation periods, hospital occupancy due to acute respiratory syndromes in older patients during flu seasons are increasing, especially in the age group over 80.
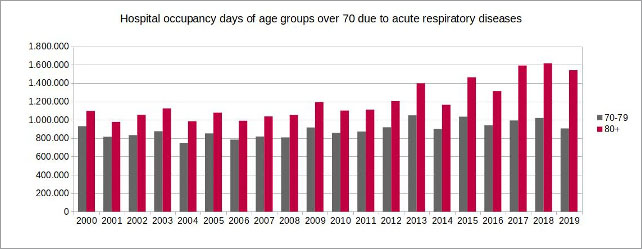
Figure 10: (click here for a larger display) Illustration by the author, data source: Federal Statistical Office
Since the groups of the early and late Elder are causing the majority of hospitalisations and because these age groups will continue to increase in the future, it is predictable that the total number of hospital occupancy days due to acute respiratory diseases will also increase.
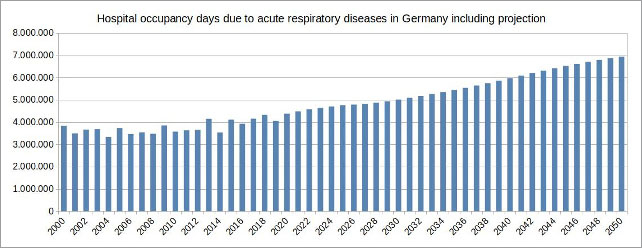
Figure 11: (click here for a larger display) Illustration by the author, data source: Federal Statistical Office
It is obvious something does not match here. On the one hand, it is comprehensible to cut down health care costs by reducing overcapacities. On the other, the challenges of an aging population can only be met in a conventional way by expanding capacities, at least during flu seasons.
Conclusion
Because of the correlation between demographic change and the resulting, expectable higher load on the health care system, it is obvious that there is a risk of a frequent overburdening, if capacities of the German health care system are further reduced and not expanded. By dramatizing the lethality of COVID-19 and the threatening overburdening of the health care system by the impact of the coronavirus, which, in fact, are both primarily due to demographic changes in the population and not to the disease, as well as focussing on a vaccine as the only solution, another, much more effective and safer alternative of disease control is kept out of the consciousness of the people: the maintenance and expansion of capacities in the health care system in order to continue to meet the requirements of an aging society in the future.
Note: The German Federal Ministry of Health has not yet responded after being addressed to reply to the correlations outlined in this article.
About the author: Karsten Montag, born in 1968, studied mechanical engineering at the RWTH Aachen, philosophy, history and physics at the University of Cologne, and educational sciences in Hagen. For many years, he was an employee of a management consulting firm with close ties to the trade unions, and most recently department and project manager in a software company that produced and distributed an energy data management and billing system for energy trading.

Diskussion
0 Kommentare